Rapidly changing and sometimes deadly viruses create critical public health risks – and a challenge for researchers working on vaccines.
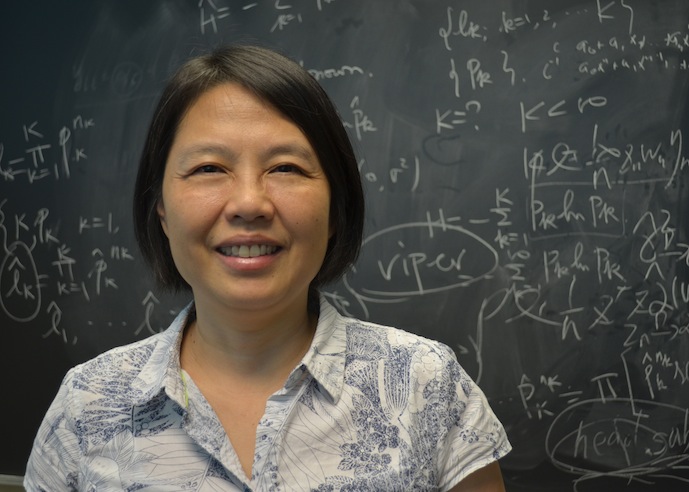
UNC Charlotte researcher Yanqing Sun has accepted that challenge. For over a decade, she has collaborated with other researchers on vaccine efficacy studies, including ones looking at HIV vaccines.
Sun primarily works with Peter Gilbert, a biostatistics researcher with Fred Hutchinson Cancer Research Center in Seattle and the University of Washington. Sun’s research specialties include developing statistical methods for analysis of event history data and longitudinal data.
“There is no known HIV vaccine that definitely works at this point,” said Sun, a statistics professor in UNC Charlotte’s Department of Mathematics and Statistics. “Scientists develop vaccines with different constructs. The vaccines are tested in the vaccine efficacy trials where the participants are randomized to receive the HIV vaccine or the placebo. We evaluate whether the vaccine works or not and how the efficacy changes. The goal is to develop more effective HIV vaccines.”
Constantly Changing Virus Complicates Development of Effective HIV Vaccine
Developing an HIV vaccine that works well has proven particularly challenging because of the constantly changing virus. Different subtypes of HIV display extreme genetic heterogeneity. This results in the same problem seen with flu vaccines, where a moderate mismatch can lead to a vaccine’s failure against specific strains of the flu. The researchers’ work holds potential implications for other viruses as well.
“Naturally, the vaccine efficacy depends on the similarity or dissimilarity between the infecting virus and a virus in the vaccine, which can be measured by some kind of distance called mark,” Sun said. “Ideally, if the vaccine is effective, then we expect that people with close virus distance will have more protection.
“However, only people who become infected will have the blood sample tested for infecting virus and will have the virus distance measured,” she said. “A further complication is that if the blood sample is measured long after the person is infected, it’s very possible the virus has already mutated.”
In this case, the observed mark is not the actual mark at the time of infection, which results in missing data or mis-measured data, she said.
“Because of the difficulties in the nature of the problem and the complications in the data collection process, we have to develop new statistical methods to accommodate all of these challenges,” she said.
New technology will enable more accurate determination as to whether the virus has mutated at the time when the blood sample is taken. But missing and/or mis-measured data is an inherent part of medical and public health studies.
Sun has been principal investigator or a co-principal investigator on numerous grants funded by the National Science Foundation and the National Institutes of Health and has over 45 publications.
“As a statistician, I would like to know that the methods developed are useful for medical and public health studies,” she said. “By working on this project for over 10 years, we’ve generated many research results. The statistical methods we developed for this research are used for the real-world applications. It’s very rewarding.”